Mastering scene size up emt: A Practical Guide
A proper EMT scene size-up isn't just a step in a protocol; it's a mindset. It’s the rapid, systematic evaluation of an emergency scene that you run before you ever make patient contact. This initial assessment, often done in less than 30 seconds, is all about keeping your crew safe, figuring out how many patients you have, getting a handle on the mechanism of injury or nature of the illness, and calling for backup if you need it.
Honestly, it's the foundation that the entire rest of the call is built upon.
Your First 30 Seconds: The EMT Scene Size Up
That first look through the ambulance windshield is everything. It's not just a view—it's the very beginning of your clinical decision-making. A solid scene size-up isn't about rigidly checking off boxes; it’s about building a dynamic mental picture of what you’re rolling into. For seasoned medics, this process starts the second the dispatch tones drop. You’re already painting a picture of the scene long before you even arrive.
This initial evaluation is so fundamental to what we do that its core components have been standardized for decades. The process was officially outlined as a key part of EMS response way back in 1994 by the U.S. Department of Transportation. The big five parts are: figuring out patient numbers, identifying the MOI/NOI, assessing resource needs, taking standard precautions (BSI), and ensuring the whole scene is safe.
Even though it’s often the quickest part of the entire patient assessment, its impact on every single action that follows is massive.
The flow from dispatch to on-scene assessment is a funnel of information, and the size-up is where it all comes together.
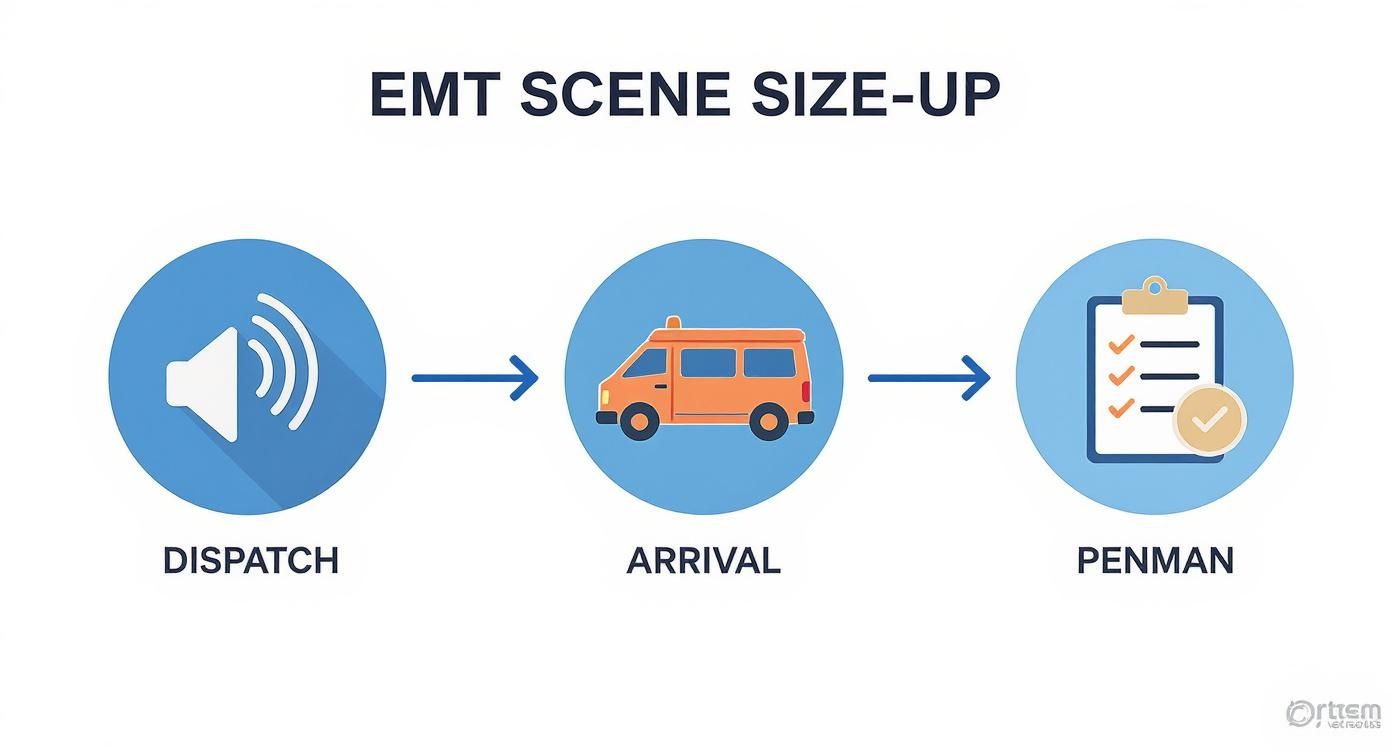
This just drives home the point that a good size-up is a structured mix of pre-arrival intel and what your own eyes are telling you right now.
The Power of a Mental Framework
When the pressure is on, our brains tend to get tunnel vision. Instead of trying to remember a laundry list of details, first responders lean on mnemonics to keep their thoughts straight. For scene size-up, the go-to tool is PENMAN.
Think of PENMAN less like a strict rulebook and more like a mental filing cabinet. It keeps you organized when the adrenaline is pumping.
- P – Personal, Partner, Patient Safety
- E – Environmental Hazards
- N – Number of Patients
- M – Mechanism of Injury / Nature of Illness
- A – Additional Resources Needed
- N – Need for Extrication / C-Spine
And this isn't a one-and-done checklist. It’s a continuous loop. You're constantly observing and re-evaluating because a scene that looks safe one second can turn dangerous in the next.
For a quick reference, here’s how the PENMAN mnemonic breaks down into practical questions and goals you should be running through your head on every call.
PENMAN Scene Size Up Mnemonic At a Glance
| Letter | Stands For | Core Question | Primary Goal |
|---|---|---|---|
| P | Personal, Partner, Patient Safety | Is the scene safe for me, my partner, and the patient? | Identify and mitigate immediate threats. |
| E | Environmental Hazards | Are there any environmental dangers (weather, terrain)? | Adapt operations to the environment. |
| N | Number of Patients | How many patients do I have? | Determine if a Mass Casualty Incident (MCI) is needed. |
| M | MOI / NOI | What happened? (Trauma vs. Medical) | Guide the initial patient assessment approach. |
| A | Additional Resources | Do I need more help (fire, law enforcement, more ambos)? | Ensure adequate resources are en route early. |
| N | Need for Extrication | Is the patient trapped? Do I need to consider C-spine? | Plan for specialized rescue and spinal motion restriction. |
Having this framework helps you quickly process a chaotic scene and make sound decisions without missing a critical piece of the puzzle.
An Actionable Example On Arrival
Let's walk through a common one: you're dispatched to a "person fell" call at a private home. As you're driving, the size-up has already begun. What time is it? Is this a neighborhood you know has safety concerns? As you pull up, you see an elderly woman sitting on the porch steps, holding her leg.
Your immediate PENMAN assessment in the first 30 seconds:
P: No obvious threats. A few neighbors are watching, but they’re keeping their distance. E: It’s a bright, sunny day, but those wooden steps look wet and slick. N: One patient visible. M: Looks like a fall from a standing position, probably a lower extremity injury. A: Probably not needed for a simple fall. N: No extrication necessary.
This rapid rundown confirms it's a relatively low-risk call. But what if you rolled up and saw a broken window and signs of a fight? Your "P" for Personal Safety would immediately change everything. You'd stage the ambulance down the street and wait for law enforcement to clear the scene.
Developing the muscle memory for this kind of rapid assessment is key. You can even find practical drills to improve reaction time that can help sharpen these critical initial moments.
Once you’ve made these decisions, clear communication is the next step. Efficiently managing your resources is just as important as identifying the need for them. This is where systems that offer dispatch and personnel tracking, like those found within the Resgrid platform, can be a game-changer.
Actionable Insight: By using a platform like Resgrid to manage personnel availability, you avoid the costly overtime that comes from calling in off-duty staff unnecessarily. You can instantly see who is on-call and available, ensuring the right resources are dispatched without over-staffing, directly saving your department money on payroll.
Prioritizing Crew Safety and Scene Control
Let's get one thing straight: the most important patient on any call is always you. We all chant "BSI, scene safe" until we're blue in the face, but a real scene size-up goes way deeper than just rattling off the words. It’s an active, non-stop process of figuring out what can hurt you and making sure it doesn't. Your number one job is to go home at the end of your shift.
Every scene throws something different at you, and your PPE is your first line of defense. But just grabbing a pair of gloves on autopilot isn't enough. Your choice of gear should be a conscious decision, one you make based on dispatch information before you even pull out of the bay.

Practical Example: You're dispatched to a "cough and fever" call at a packed apartment building during flu season. This screams for a higher level of caution. An N95 and eye pro should be on your mind before you step out of the truck. Compare this to a "fall at a construction site," which probably just needs gloves and maybe safety glasses. This proactive thinking saves precious time and cuts down your risk of exposure.
Using Your Environment for Protection
That ambulance you're driving is more than just a ride to the hospital; it's a 6,000-pound piece of safety equipment. When you're on a highway for an MVC, where you park that rig is everything.
Positioning the ambulance upstream of the wreck, at an angle, creates a solid physical barrier between your crew and the cars still flying down the road. This "fend-off" position can be the one thing that prevents a secondary collision from taking out responders. It's a non-negotiable.
But it's not always about the big, obvious dangers. The subtle, environmental threats are often the ones that get you because they're so easy to miss.
- Spot the Ice: On a cold morning, that dark patch on the asphalt might not be a puddle. Assume every wet-looking spot is black ice until you know for sure. A slip and fall can take you out of commission just as easily as a major accident.
- Scan for Hidden Traffic: A quiet residential street can feel safe, but it’s full of blind corners and hidden driveways. Never assume drivers see you. Keep your head on a swivel.
- Identify Downed Lines: Never, ever, approach a vehicle with a power line draped over it. It doesn't have to be sparking to be live. Set up a big danger zone and wait for the utility company to give the all-clear. Period.
The rookie mistake is getting tunnel vision and rushing straight to the patient. Force yourself to take three extra seconds to scan your surroundings. That discipline is what separates a seasoned vet from a new EMT.
Recognizing Behavioral and Chemical Threats
Not all threats are things you can trip over. Sometimes, the danger is in how people are acting. As you approach, clock the bystanders. Are they agitated? Is your patient clenching their fists or pacing? These are pre-attack signals. If your gut screams that a scene feels wrong, it probably is. Don't be a hero—stage a few blocks away and call for law enforcement to make it safe first.
Practical Example: You respond to a semi-truck rollover on the interstate. As you approach, your eyes should immediately be looking for placards. Those little diamond-shaped signs tell you what you're dealing with. Seeing a "1203" placard (gasoline) means you stage upwind and uphill, call for the HazMat team, and prevent a potential explosion. Ignoring that placard could be a fatal error.
This level of detailed observation is crucial, but it's useless if you keep it to yourself. Keeping your entire team in the loop as the scene evolves is where modern tools really shine.
Actionable Insight: The messaging features in Resgrid's mobile applications allow crews to share real-time updates on scene conditions. A quick message like "Unstable structure, use east entrance only" can prevent injuries and costly workers' comp claims. This simple communication standardizes safety info, turning a personal task into a rock-solid, team-wide shield.
Reading the Scene: The MOI and NOI
Every emergency scene tells a story. Long before you ask a single question, the environment itself is giving you clues about your patient's condition. This is where a good EMT becomes a great one. For trauma calls, you’re a detective, piecing together the Mechanism of Injury (MOI). On medical calls, you’re a profiler, figuring out the Nature of Illness (NOI) from subtle hints scattered around the room.
Getting this part of the scene size-up right saves precious time. An accurate first read means you’re grabbing the right gear from the truck on the first trip, not the second or third. It means you’re already thinking about whether you’ll need a trauma center or a specific medication, which makes the whole call run smoother.

This process is so fundamental that starting in April 2025, "Scene Size-Up" will make up 15–19% of the NREMT cognitive exam. They’re serious about this, and so should you be.
Decoding the Mechanism of Injury
The MOI is just a technical way of asking, "How did energy hit the body and cause damage?" It's physics, plain and simple. When you roll up on a car crash, you aren't just looking at a mess of twisted metal; you're looking for evidence of what happened to the people inside.
Practical Example: A bent steering wheel isn't just a part of the car. It screams "high-energy impact to the driver's chest." Instantly, your index of suspicion for a collapsed lung, a bruised heart, or fractured ribs should go through the roof. That one observation means you’re already prepping for shock and breathing problems before you’ve even laid a hand on your patient.
Keep an eye out for these classic MOI clues:
- "Starburst" Windshield: That spiderweb pattern means a head hit the glass. Assume a head injury and, just as importantly, a cervical spine injury until you can prove otherwise.
- Driver's Side Intrusion: If the car door is caved into the passenger compartment, you can bet there are injuries on that side of the body. Start thinking about a fractured pelvis, internal bleeding in the abdomen, or a busted spleen or liver.
- Ejection from Vehicle: This one’s easy. A patient thrown from a car is an automatic high-priority trauma. Assume they have multiple, severe injuries. Period.
An experienced medic knows that identifying a high-energy MOI early saves time and money. It's the justification you need to call for an ALS intercept or get a helicopter spinning up sooner rather than later. A false activation is way cheaper than the clinical—and financial—cost of delaying definitive care for a critical patient.
Uncovering the Nature of Illness
With medical calls, the NOI is usually a bit more subtle. You have to hunt for clues in the patient's environment to build a working diagnosis, especially when your patient is too confused or breathless to give you a straight answer.
Picture this: you get dispatched for an "unresponsive person." As you step into the living room, what do you see?
Practical Example A: The Diabetic Emergency
You scan the room and see a glucometer and a logbook on the coffee table. Next to it, there’s a half-eaten meal and a bottle of insulin. Your brain should immediately jump to a hypoglycemic event. You know to grab your glucometer and D50 before you do anything else.
Practical Example B: The Potential Overdose
Same call, different scene. This time, you spot prescription pill bottles on the nightstand—some empty, some recently filled. Maybe you see drug paraphernalia. This paints a picture of a likely overdose, pushing you to prepare naloxone and focus on managing their airway.
The clues aren't always so obvious. A messy home with overflowing trash and mail piling up might suggest a patient with a chronic illness who hasn't been able to care for themselves. That's a huge hint that you could be dealing with dehydration, infection, or other ugly complications.
Putting It All Together
Analyzing the MOI and NOI isn't a one-and-done task. It's a continuous process that starts with the dispatch information, continues with your windshield survey, and sharpens as you get closer to your patient.
Honing this skill is a massive cost-saver for any agency. By predicting injuries and illnesses, you:
- Reduce Wasted Supplies: You bring in only what you need, not the entire contents of the ambulance.
- Optimize Personnel: You know if you need to call for ALS or specialized rescue early, cutting down on-scene delays.
- Ensure Proper Destination: Identifying a stroke patient (NOI) or major trauma (MOI) helps you justify transport to a specialty center from the get-go, avoiding time-consuming and costly hospital transfers.
Ultimately, reading the scene is about being proactive. You’re not just reacting to what you find; you’re using the evidence in front of you to predict what’s coming next.
Counting Patients and Calling for Resources
It's one of the easiest and most dangerous traps to fall into during a scene size up emt: getting tunnel vision. You roll up, see the one patient who's screaming or obviously hurt, and your entire focus narrows down to just them. That kind of hyper-focus can make you completely miss other victims—the ones who are quiet, maybe unconscious, and often in much worse shape.
Practical Example: On a nighttime MVC, you must force yourself to do a slow, 360-degree scan with a high-powered flashlight. Look past the immediate wreckage. Are there signs of ejection, like a shoe or a cell phone thrown fifty feet from the wreck? Shine the light into the woods and ditches. Remember: a quiet patient is often a sick patient.

This methodical scan isn't just about finding people; it’s about building an accurate patient count. That number is the absolute cornerstone of managing your scene. Get it wrong, and your crew gets overwhelmed fast, meaning somebody's not getting the care they need.
Making the Call for Backup
Once you have that patient count, the next question is immediate: Do I have enough help? And the answer isn't just about raw numbers. It's about acuity. One combative patient can tie up more responders than two cooperative ones. A single critical trauma patient can require your entire crew's attention.
And don't just think in terms of calling another ambulance. A good size-up considers every possible need on the board.
- Law Enforcement: You need them for crowd control, shutting down traffic, or any scene that just feels off. If the hair on your arms is standing up, they should be rolling.
- Fire Department: They're your go-to for vehicle extrication, fire suppression, or hazmat, but don't forget they're also great for extra hands when you've got a heavy lift in an awkward spot.
- Specialized Resources: This could be anything from a helicopter for a remote scene with a long ground transport to a bariatric unit for a patient you can't safely move on your own.
There's a golden rule here, and it's simple: It is always, always better to call for help early and cancel it than to call for it late when you're already in the weeds. A canceled unit is a minor inconvenience. A delayed response for a critical patient can be a catastrophe.
Practical Scenarios for Resource Allocation
Let’s put this into practice. Dispatch sends you to a "vehicle versus pedestrian." You arrive and see one patient down and a frantic, yelling driver pacing on the sidewalk.
Your first instinct might be that your two-person crew can handle one patient. But a better size-up tells a different story. That agitated driver? He's a potential safety risk. The crowd starting to form? They could get in your way. Now you need law enforcement for scene control. Oh, and the patient is pinned under the car's front tire. That means you need the fire department for a lift assist. All of a sudden, your "one-patient call" requires three different agencies.
This is why having more people on scene just plain works. Field studies have shown that crews with three or four responders get to and extricate patients significantly faster than two-person crews. We're talking about accessing patients around 30 seconds faster and completing removal 1.2 to 1.5 minutes sooner. In major trauma or cardiac arrest, those are the minutes that make all the difference.
Saving Money by Thinking Ahead
Calling for the right resources early isn't just good medicine; it's good economics. A chaotic, under-resourced scene is where mistakes happen, delays mount, and patient outcomes suffer—all of which have downstream financial costs. When you get the right people and equipment on the way from the jump, you create a controlled, efficient environment.
Actionable Insight: A platform like Resgrid saves money by preventing unnecessary resource deployment. Instead of blindly calling for multiple units, you can use the system to broadcast a need and have available, nearby units respond. This "pull" model is far more efficient than a "push" model, reducing fuel costs, vehicle wear-and-tear, and the cost of pulling units away from their primary coverage areas. If you ever need help configuring your dispatch or resource-calling protocols, you can find some great guidance over at the https://resgrid.com/support.
Avoiding Common Pitfalls in Your Size Up
On any call, complacency is your silent, unwelcome partner. It doesn't matter if you're a fresh EMT or a 20-year veteran; the real danger often isn't the roaring fire or the mangled car. It's the routine call—the simple "person fell" dispatch that might be masking a domestic violence situation, or the "fender bender" that hides a patient ejected deep into the woods.
This is where a disciplined, consistent scene size-up becomes your most critical skill. It’s not just a box you check off in school. It’s a career-long habit that forces you to challenge assumptions and see what's really in front of you. Falling into these common traps doesn't just create chaos; it can get your crew hurt and delay care for the people who need you most.
https://www.youtube.com/embed/-j1ycX_4org
The Danger of Tunnel Vision
By far, the most common mistake is getting laser-focused on the first, most obvious patient. You pull up to a two-car wreck, and the driver of one vehicle is leaning on the horn, screaming. Every instinct tells you to run to them. But that "squeaky wheel" can easily pull your attention from a much more critical patient—the silent, unconscious occupant in the other car.
To fight this, you have to force a deliberate pause. Before you even open the ambulance door, take three slow, deep breaths and do a methodical 360-degree scan of the entire scene.
- Look Beyond the Obvious: Are there signs of another vehicle down an embankment? Check under cars, in ditches, and behind bushes.
- Listen for the Unseen: Can you hear faint cries for help over the noise?
- Account for Everyone: If a bystander says a car had three occupants but you only see two, you have a missing patient until you prove otherwise.
A veteran medic once told me, "The quiet ones are the ones that will kill you—and the ones you'll kill if you miss them." That advice has stuck with me. A loud patient is breathing; a quiet one might not be.
Ignoring Your Gut Feeling
Sometimes, a scene just feels wrong. The story doesn't quite match the injuries you're seeing. A bystander seems a little too interested in your gear. The house is eerily quiet when it should be chaotic.
Ignoring that internal alarm is a massive mistake. That feeling is your subconscious picking up on thousands of tiny cues that your conscious mind hasn't pieced together yet. If a scene feels unsafe, it is unsafe until proven otherwise.
Practical Example: You respond to a "man down" call. You arrive to find the front door ajar, but no one answers your calls. Your gut tells you something is off. Don't just barge in. Stage your ambulance a block away, advise dispatch you're waiting for law enforcement, and let them clear the home first. A few minutes' delay is infinitely better than your crew becoming part of a crime scene.
Special Considerations for Vulnerable Patients
In a chaotic environment, kids and the elderly are frequently overlooked or mis-triaged. Their unique physiology and potential communication barriers make them tough to assess in a hurry.
- Pediatric Patients: Kids are small and can be easily hidden from view in a wreck. They also have a frustrating ability to compensate physiologically for a long time before crashing suddenly. A child who looks "stable" is always a high priority.
- Geriatric Patients: An elderly person's fall might not be just a simple trip. The nature of illness could be a serious medical event like a stroke or heart attack that caused the fall. Don't just treat the scraped knee; the NOI might be far more serious than the MOI suggests.
Getting this right is not just good practice; it's a huge part of your certification. The initial evaluation accounts for a significant portion of national exams, from 15% to 23% of the test content. The NREMT's EMT exam, for instance, dedicates 15%-19% of its questions to this domain because it's the foundation for everything that follows. You can explore the detailed breakdown of NREMT exam content to see just how critical this skill is considered.
Navigating Potential Crime Scenes
What happens when you walk into a scene and immediately suspect criminal activity? Your priority is always patient care, but you also have a duty to not trample all over the evidence.
- Be Observant: Mentally note the position of furniture, weapons, or shell casings.
- Touch Only What's Necessary: Don't move anything unless it's directly preventing you from reaching or treating your patient.
- Communicate with PD: When law enforcement arrives, tell them what you saw and what you had to move. A simple statement like, "We found the patient on the floor over there, and we had to cut their shirt off," helps them piece the scene back together.
Preserving evidence while doing your job shows professionalism and builds a strong working relationship with law enforcement. Trust me, that pays off on future calls.
Scene Size-Up Mistake vs. Expert Action
Even seasoned providers can fall into bad habits. The key is to recognize these pitfalls and consciously choose a better course of action. This table breaks down some of the most common errors and contrasts them with the mindset of an expert provider.
| Common Pitfall | Description of Error | Expert Corrective Action |
|---|---|---|
| Tunnel Vision | Rushing directly to the loudest or most obvious patient without assessing the entire scene first. | Perform a deliberate 360-degree scan from the vehicle before exiting. Prioritize the quiet patients first. |
| Ignoring Intuition | Dismissing a "gut feeling" that a scene is unsafe because there's no immediate, obvious threat. | Treat that feeling as valid data. Stage a safe distance away and request law enforcement to secure the scene. |
| Assumption of Safety | Believing a scene is safe just because dispatch didn't mention any hazards. "Man down" could mean anything. | Assume every scene is unsafe until you can prove otherwise. Actively look for hidden dangers. |
| Forgetting Resources | Trying to manage a multi-patient incident alone or with a single crew, leading to delays and chaos. | Call for backup early and often. It's always better to send resources home than to need them and not have them. |
| Neglecting the NOI | Focusing only on the traumatic injury (MOI) and missing an underlying medical cause (NOI), especially in falls. | Always ask "why" the event happened. Could a medical issue like a syncopal episode have caused the fall or crash? |
| Poor Communication | Failing to give a clear, concise initial report to dispatch, leaving incoming units in the dark. | Provide a quick, standardized report (e.g., "Medic 1 on scene, two-car MVC, two visible patients, requesting one additional unit."). |
Ultimately, avoiding these pitfalls comes down to discipline. It's about fighting complacency on every single call and treating the scene size-up not as a preliminary step, but as the most important one you'll take. It sets the tone for the entire encounter and is the first, best line of defense for you, your partner, and your patient.
EMT Scene Size-Up FAQs
Stepping off the truck for your first few calls is a big deal. The textbook checklists are one thing, but figuring out how they apply when the adrenaline is pumping is another. Let's tackle some of the most common questions new EMTs have about the real-world scene size-up.
How Long Should a Scene Size-Up Actually Take?
You can forget about the stopwatch. The initial windshield survey and the first few seconds you're out of the rig? That should all happen in the first 30 to 60 seconds. But here's the key: the size-up never really ends.
Practical Example: A simple medical call for a stubbed toe is going to have a lightning-fast initial size-up. But a multi-car pileup on the highway? That requires a continuous, evolving size-up as more units arrive, new hazards pop up (like a fuel leak), and the situation changes. The goal isn't speed; it's being thorough and staying safe.
The best scene size-up is a constant loop of observing and re-evaluating. A scene that was perfectly safe three minutes ago can turn dangerous in a heartbeat. You have to keep your head on a swivel for the entire call.
What Is the Most Overlooked Part of the Scene Size-Up?
Easy. It's underestimating the need for more help. So many new providers get tunnel vision on the first patient they see and try to be heroes, managing way too much with a single crew. Not only is it a recipe for burnout, but it's also flat-out unsafe.
Practical Example: Your crew of two is called for an elderly person who fell. You arrive to find a 400lb patient on the floor in a cramped bathroom. There is no physical way the two of you can safely lift and extricate them. Trying to do so risks a career-ending back injury. The correct move is to immediately call for a lift assist from the fire department.
Calling for backup early and then canceling them if you don't need them is the cheapest insurance policy you'll ever find. It shows good judgment, not weakness, and prevents costly on-the-job injuries.
How Do You Handle a Chaotic or Loud Scene?
When things get loud and chaotic, every instinct will scream at you to hurry up. You have to fight that urge and consciously slow down. In a high-stress environment, your eyes are far more reliable than your ears.
- Filter the Noise: Don't just hear the chaos; see what's causing it. Are people running toward the scene or fleeing from it? Is that smoke from a fire or just dust from a collapse?
- Create a Barrier: Use your ambulance. It's a giant, heavy piece of metal. Park it strategically to create a physical safe zone between your crew and threats like traffic or an unruly crowd.
- Trust Your Gut: This is a big one. If a scene just feels wrong, it probably is. There's no shame in staging a block away, keying up the mic to advise dispatch, and waiting for law enforcement to give the all-clear. Never, ever enter a scene until you're certain it's safe.
What if the Scene Becomes Unsafe After Making Contact?
Your safety comes first. Your partner's safety comes first. That's it. Full stop. If a scene goes south after you've already started patient care, you get out.
Yell the threat clearly to your partner—"He's got a knife, we're out!"—and move. Don't worry about the equipment. Grab your portable radio and jump kit only if you can do it without a moment's hesitation. Get back to the truck, lock the doors, and immediately notify dispatch of the situation and request police. You can't help anyone if you become a patient yourself.
Here at Resgrid, we know that a solid scene size-up is the foundation of every successful call. Our platform is built to help you manage that scene, giving you the tools to coordinate personnel, dispatch units, and share real-time updates so your team has the support it needs from the very first moment. Find out more at https://resgrid.com.

